Spindle Cell Melanoma : A Case Report
Anjana AK1, P Muraleedharan Nampoothiri1, Abdul Manaf1, Sandeep Sreedhar1
1. Department of Otorhinolaryngology, Malabar Medical College and Research Centre, Kozhikode kerala, India*
Corresponding Author: Dr Anjana AK
Department of Otorhinolaryngology, Malabar Medical College and Research Centre, Kozhikode kerala, India Email: anjoozanju61@gmail.com
ABSTRACT
Spindle cell melanoma (SCM) is a subtype of melanoma which is rare and exclusively composed of spindle cells.This genetically represents a diverse group of melanomas .It mainly involves head,neck and trunk.Here we report a case of 22 year old female patient with spindle cell melanoma from the Northern kerala ,initially misdiagnosed as “Granulomatous Lymphadenitis” which was the main diagnostic challenge. Her clinical, radiological histopathological and immunohistochemical are mentioned in the report out of which immunohistochemistry clutched the diagnosis.
Keywords: Spindle cells, S100, SOX10, Metastatic Melanoma
BACKGROUND
Spindle cell Melanoma (SCM) is rare type of malignant melanoma composed of spindled neoplastic cells arranged in sheets and fascicle. Lack of expression of several melanoma markers makes the diagnosis as very challenging.1
SCM may occur anywhere on the body and frequently mimics amelanotic lesions, including scarring and inflammation. Histological cytologic features of SCM are indistinct and confused with other epithelial neoplasm including sarcoma and lymphoma.2-5 SCM is typically encountered as a primary cutaneous lesions but it may occasionally present with lymph nodal involvement.6 Like Interdigitating cell sarcoma, Intranodal SCM has variable morphological appearance and may contain both fusiform and epithelial cells. Intralesional melanin pigment is only exceptionally present in SCM, but interspersed lymphocytes and mitotic activity is common. SCM is unique melanoma variant because it is almost always lacks “specialized melanocyte’’ determinants such as HMB -45, Melanin A, PNL1, Tyrosinase and only rarely manifests the production of melanin. Tumour shows restricted reactivity for S100 protein,Vimentin and CD 68.7-9 P75 is also reported in SCM. Immunophenotypic features of SCM and ICDS appear to be indistinguishable from one another. SCM and IDCS belong to those lesions which share morphologic and immunohistochemical features. Molecular analysis for BRAF aberrations had shown examples of both IDCS and SCM that had V600E or V600R mutation. BRAF mutation is commonly found in pure spindle cell type melanoma and also due to financial implications, very difficult to test.10-12
CASE PRESENTATION
22 year female who is a working woman came with complaints of painless left sided neck swelling for 1 month which was initially small in size later progressed. She had a history of hypothyroidism. She was otherwise asymptomatic. There was no history of fever, loss of weight or decrease in appetite. General examination was found to be within normal limits.
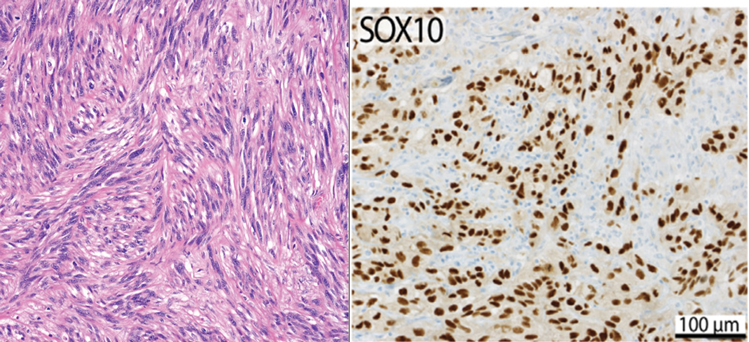
Figure 1. H&E of SCM and pathology outline of SOX10
Physical examination – On inspection, a swelling of size 1x2 cm size in the left lower part of neck was noted with no scar/sinus /dilated veins and visible pulsations. The skin over the swelling found to be normal. On palpation – swelling of 1x1 cm noted in anterior triangle of neck that was non tender with no local rise of temperature. Surface is nodular, vertically mobile and horizontally restricted mobility, firm in consistency and less prominent on neck extension and medial to sternocleidomastoid. No other swelling seen in any part of neck and body.
Fine needle aspiration cytology report of neck mass revealed granulomatous lymphadenitis and suggested excision of lymphnode for further assessment. USG neck shows well defined heterogeneous hypoechoic lesion in the left side of neck suggestive of schwannoma. Computed Tomography scan of neck showed a well defined fusiform heterogeneously enhancing lesion measuring 43x26x17 mm with cystic area noted in left level IV abutting left IJV medially and sternocleidomastoid anteromedially. There is non enhancing areas within the lesion – S/O necrosis with no evidence of calcification/sinus formation.
Surgical excision of neck mass was performed 1 week later after FNAC and specimen sent for Histopathological examination. Histopathology section showed spindle to ovoid cells arranged as long and short fascicles, whorls, nests and storiform pattern with focal lobulated areas. Mild to moderate nuclear atypia noted with few binucleated /multinucleated cells and bizarre forms and cells with horse shoe /kidney shaped nucleus seen. It was suggestive of spindle cell neoplasm and advised to do a panel of Immunohistochemistry. Immunohistochemistry was done and strongly and diffusely + ve for S100.

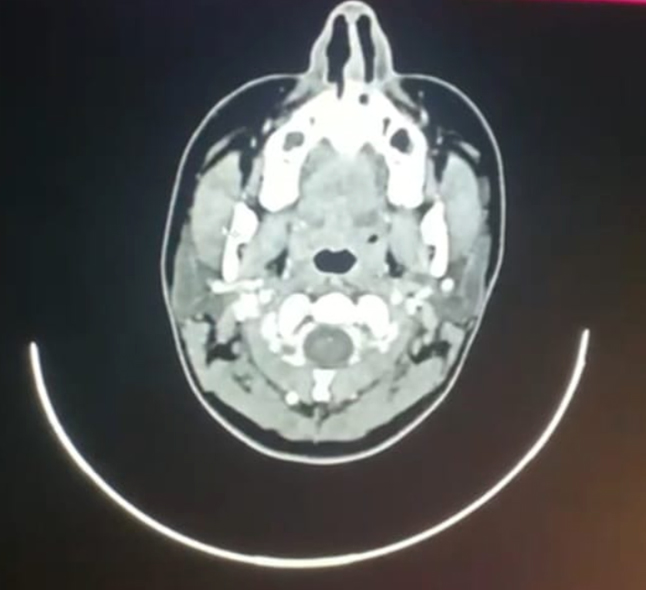
Figure 2. CT neck sagittal and axial view
Patient was referred to higher centre for further treatment. F-18 FDG PET /CT study was done from there as follow up to detect any residual or recurrent disease and there was no evidence of clinically significant abnormal hypermetabolism anywhere in the body. Repeated Histopathological examination showed circumscribed lesions comprising interconnected broad fascicles of medium sized spindle cells in a dense lymphoid stroma and spindle cells have high NC ratio with oval/spindled blunt ended nuclei with vesicular chromatin and scanty cytoplasm. The Tumour cells express S100 protein, SOX 10, HMB -45 (weak) and MiTF and are immunonegative for CD1a, Langerin, Fascin, CD35, Melanin A and CD 68 and was diagnosed as Metastatic spindle cell melanoma. Left Modified Radical Neck Dissection was done later after obtaining necessary fitness. Later Histopathology report showed negative for metastasis for level Ia and Ib lymphnodes,with metastatic tumour without extranodal extension for level II,III,IV enbloc.
DISCUSSION
Our report is a rare case of spindle cell melanoma lately diagnosed. The importance of tissue biopsy is highlighted here, which helped to clinch the diagnosis. Of all the melanoma cases, SCM is rare and reported incidence between 3 and 14%.13 As there is chance of metastasis, SCM cases should be monitored carefully. Differential diagnosis for spindle cell melanoma includes spindle cell nevus, desmoplastic melanoma, dermatofibrosarcoma.1
ABCDE method (Assymetry, border irregularity, colour variation diameter and Evolution) has been employed for diagnosis classically in the case of melanoma, but for more rare subtypes like nodular and desmoplastic melanoma, these are insufficient.
By Histopathological Examination, these diagnosis can be differentiated. Here, SOX -10, S100 positivity supports the diagnosis of malignant melanoma. However in this case, there is no overlying skin changes. They does not express other melanocyte markers like HMB 45 and Melanin A. So to achieve accurate diagnosis we need a panel of immunohistochemistry as there can be cytological atypia. Other markers like KP1positively stains for most B cell NHL and CD163 is specific marker for Histiocytic sarcoma
Melanoma is a common malignancy that occurs over a wide range of age. It is also notorious for its strong tendency to metastasize to virtually any site within the body and at any time after the primary tumour has been discovered.14 Fine-needle aspiration (FNA), a simple, fast, minimally invasive, and cost-effective procedure, is often used as an initial diagnostic tool in the evaluation of suspected metastatic or recurrent disease. Characteristic cytologic features normally varies from elongated to rounded with a moderate amount of amophilic cytoplasm with hypercellular aspirates, dispersed cellular distribution, epithelioid or plasmacytoid cells with eccentric nuclei, cytoplasmic melanin pigments, intranuclear pseudoinclusions, macronucleoli, and binucleation or multinucleation.15-17 In contrast, in this case, histopathology sections showed spindle to ovoid cells arranged as long and short fascicles, whorls, nests and storiform pattern with focal lobulated areas. Mild to moderate nuclear atypia noted with few binucleated /multinucleated cells and bizarre forms and cells with horse shoe /kidney shaped nucleus seen. S100 is sensitive marker that labels primary and metastatic melanoma including the spindle cell variant.18 Full awareness of FNA features of spindle cell melanoma and findings of panel of immunohistomarkers will be helpful in diagnosing metastatic spindle cell melanoma by FNA.19
CONCLUSION
Spindle cell melanoma is defined by presence of spindle shaped melanocytes and is a rare histological variant of melanoma. There is no exact cause known. This is often misdiagnosed and need histological clues and immunohistochemistry to make correct diagnosis.20 We report a rare case of spindle cell melanoma originally mistaken for granulomatous disease. Initially excision biopsy was done and sent for histopathological examination. Later Modified radical neck dissection was done showed negative for metastasis for level Ia and Ib lymphnodes, with metastatic tumour without extranodal extension for level II, III, IV enbloc. Spindle cell Melanoma requires a high index of suspicion and IHC for spindle cell lesions, even with atypical presentations.
END NOTE
Author information
- Dr. Anjana AK, Department of Otorhinolaryngology, Malabar Medical College and Research Centre, Kozhikode kerala, India
E-mail: anjoozanju@gmail.com - Dr P Muraleedharan Nampoothiri, Department of Otorhinolaryngology, Malabar Medical College and Research Centre, Kozhikode kerala, India
Email: pmnamboothiri@yahoo.com - Dr Abdul Manaf, Department of Otorhinolaryngology, Malabar Medical College and Research Centre, Kozhikode kerala, India
Email: manafclct@gmail.com - Dr Aju Ravindran, Department of Otorhinolaryngology, Malabar Medical College and Research Centre, Kozhikode kerala, India
Email: sreedhar.sandeep@gmail.com
Declaration: Ethics approval and consent to participate : Not applicable
Consent for Publication: Consent for publication was obtained from patient presented in this submission
Availability of data and materials: Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study
Competing interests: The authors declare that they have no competing interests
Funding: No funding was received for this submission
Acknowledgements: We would like to acknowledge the department of ENT for their support on this project and the patient who have given the full details
REFERENCES
- Winnepenninckx V, De Vos R, Stas M, van den Oord JJ. New phenotypical and ultrastructural findings in spindle cell (desmoplastic/neurotropic) melanoma. Appl Immunohistochem Mol Morphol. 2003 Dec;11(4):319–325.
[Pubmed] - Jackson CR, Minca EC, Kapil JP, Smith SC, Billings SD. Superficial malignant peripheral nerve sheath tumor with overlying intradermal melanocytic nevus mimicking spindle cell melanoma. J Cutan Pathol. 2016;43(12):1220–1225.
[Pubmed] - Walia R, Jain D, Mathur SR, Iyer VK. Spindle cell melanoma: comparison of cytomorphological features with the epithelioid variant. Acta Cytol. 2013;57(6):557–561.
[Pubmed] - Falconieri G, Bacchi CE, Luzar B. Cutaneous clear cell sarcoma: report of three cases of a potentially underestimated mimicker of spindle cell melanoma. Am J Dermatopathol. 2012;34(6):619–625.
[Pubmed] - Yeh I, Vemula SS, Mirza SA, McCalmont TH. Neurofibroma-like spindle cell melanoma: CD34 fingerprint and CGH for diagnosis. Am J Dermatopathol. 2012;34(7):668–670.
[Pubmed] - Stowman AM, Mills SE, Wick MR. Spindle cell melanoma and interdigitating dendritic cell sarcoma. Am J Surg Pathol. 2016;40(9):1270–1279.
[Pubmed] - Gloghini A, Rizzo A, Zanette I, et al. KP1/CD68 expression in malignant neoplasms including lymphomas, sarcomas, and carcinomas. Am J Clin Pathol. 1995;103(4):425–431.
[Pubmed] - Longacre TA, Egbert BM, Rouse RV. Desmoplastic and spindle-cell malignant melanoma: an immunohistochemical study. Am J Surg Pathol. 1996;20(12):1489–1500.
[Pubmed] - Pernick NL, DaSilva M, Gangi MD, et al. “Histiocytic” markers in melanoma. Mod Pathol. 1999;12(11):1072–1077.
[Pubmed] - Di Liso E, Pennelli N, Lodovichetti G, et al. BRAF mutation in interdigitating dendritic cell sarcoma: a case report and review of the literature. Cancer Biol Ther. 2015;16(8):1128–1135.
[Pubmed] - Go H, Jeon YK, Huh J, et al. Frequent detection of BRAF V600E mutations in histiocytic and dendritic cell neoplasms. Histopathology. 2014;65(2):261–272.
[Pubmed] - Kim J, Lazar AJ, Davies MA, et al. BRAF, NRAS and KIT sequencing analysis of spindle cell melanoma. J Cutan Pathol. 2012;39(9):821–825.
[Pubmed] - Gupta SK, Rajwanshi AK, Das DK. Fine-needle aspiration cytology smear patterns of malignant melanoma. Acta Cytol. 1985 Nov–Dec;29(6):983–988.
[Pubmed] - Schmid-Wendtner MH, Baumert J, Schmidt M, et al. Late metastases of cutaneous melanoma: analysis of 31 patients. J Am Acad Dermatol. 2000;43(4):605–609.
[Pubmed] - Woyke S, Domagala W, Czerniak B, et al. Fine-needle aspiration cytology of malignant melanoma of the skin. Acta Cytol. 1980;24(6):529–538.
[Pubmed] - Nasiell K, Tani E, Skoog L. Fine-needle aspiration cytology and immunocytochemistry of metastatic melanoma. Cytopathology. 1991;2(3):137–147.
[Pubmed] - Murali R, Doubrovsky A, Watson GF, et al. Diagnosis of metastatic melanoma by fine-needle biopsy: analysis of 2,204 cases. Am J Clin Pathol. 2007;127(3):385–397.
[Pubmed] - Kapila K, Kharbanda K, Verma K. Cytomorphology of metastatic melanoma: use of S-100 protein in diagnosis of amelanotic melanoma. Cytopathology. 1991;2(4):229–237.
[Pubmed] - Piao Y, Guo M, Gong Y. Diagnostic challenges of metastatic spindle cell melanoma on fine-needle aspiration specimens. Cancer. 2008;114(2):94–101.
[Pubmed] - Weissinger SE, Keil P, Silvers DN, et al. A diagnostic algorithm to distinguish desmoplastic from spindle cell melanoma. Mod Pathol. 2014;27(4):524–534.
[Pubmed]