Primary Laryngeal Amyloidosis – A Case Report
Anita Elza Thomas1, Sapna. S. Nambiar2, Hasila Beegum1, Amina Rajan1
1.Junior Resident, Department of ENT, Government Medical College Kozhikode;
2. Additional Professor, Department of ENT, Government Medical College Kozhikode*
Corresponding Author: Dr. Anita Elza Thomas, Junior Resident,
Department of ENT, Government Medical College Kozhikode
Address : Ponnasseril Suja Cottage, Pallickal, Kayamkulam, Alappuzha – 690503
Email ID : anitaelzathomas@gmail.com Phone number : 9048043033
ABSTRACT
Dysphonia is a common symptom in otolaryngology, usually linked to benign or functional causes, but it can rarely be the sole presentation of infiltrative conditions such as laryngeal amyloidosis, often leading to misdiagnosis due to nonspecific clinical and radiologic features.
We report a 60-year-old woman with three months of progressive dysphonia without airway or systemic symptoms. Laryngoscopy revealed yellowish submucosal polypoidal lesions over the right vestibular band and both vocal cords, and neck imaging showed enhancing supraglottic lesions. She underwent CO₂ laser–assisted microlaryngoscopic excision, allowing precise removal with mucosal preservation. Histopathology confirmed amyloidosis, and systemic workup ruled out generalized disease, establishing primary localized laryngeal amyloidosis. Postoperatively, the patient experienced marked improvement in voice quality and remains disease-free on follow-up.
This case underscores the need to consider rare etiologies in isolated dysphonia and highlights CO₂ laser excision as an effective treatment providing excellent functional outcomes.
Keywords: Laryngeal amyloidosis, Dysphonia, CO₂ laser, Submucosal laryngeal lesion, Congo red stain, Amyloid
Introduction
Dysphonia, while a frequent and often innocuous symptom, can occasionally herald a rare and diagnostically challenging condition. Among these, primary localized laryngeal amyloidosis (PLLA) stands as an enigmatic entity—rare, chronic and indolent in presentation characterised by the extracellular deposition of fibrillar amyloid proteins within the laryngeal framework. First reported by Burow and Neumann in 1875, laryngeal amyloidosis remains a diagnostic puzzle owing to its protean presentation and non-specific imaging findings.1
Comprising only 0.2–1.2% of benign laryngeal tumours, PLLA is most commonly encountered in males between the fifth and seventh decades of life.2,3 Unlike systemic amyloidosis, which portends a grim prognosis, localized forms are typically benign yet prone to recur frequently. Amyloid deposition within the larynx most commonly involves the false vocal cords, true vocal cords and aryepiglottic folds.3–5
Dysphonia, a consequence of vibratory disruption at the glottis, is usually the sentinel symptom. However, given its ubiquity in more common benign conditions, amyloidosis often evades early diagnosis.2,6 We report a case where isolated hoarseness of voice was the sole finding and a high index of suspicion on clinical examination led to the revelation of this rare disease with an update on the nuances of its modern diagnostic and therapeutic management.
Case Report
A 60-year-old woman was referred to our outpatient ENT clinic with a three-month history of gradually progressive hoarseness of voice. The patient described her voice as breathy, low-pitched with poor projection. She denied any associated pain, throat discomfort, dyspnoea, stridor or dysphagia. There was no history of recent upper respiratory tract infection, voice abuse, trauma or systemic illness. She was a non-smoker and did not consume alcohol.
Physical examination revealed no cervical lymphadenopathy or palpable masses. Video laryngoscopy identified multiple yellowish polypoidal lesions involving the right vestibular band, posterior one-third of the right vocal cord, and anterior two-thirds of the left vocal cord. The lesions appeared firm, submucosal and non-ulcerative, with preserved bilateral vocal cord mobility (Figure1).

Figure 1. Videolaryngoscopic image showing yellowish polypoidal lesions involving right vestibular band and bilateral vocal cords
A CECT of the neck showed heterogeneously enhancing soft tissue lesions in the supraglottic and glottis regions with no evidence of calcification, necrosis, or regional lymphadenopathy (Figure 2).
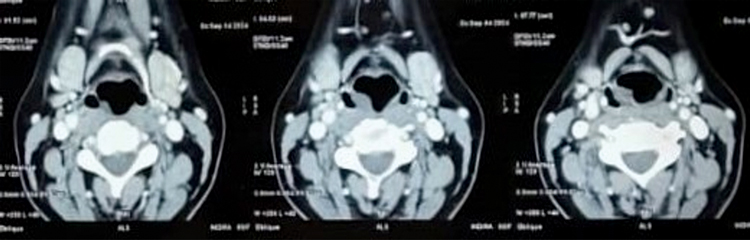
Figure 2. CECT Neck showing heterogeneously enhancing soft tissue lesions in the supraglottis and glottis
Routine haematological and biochemical profiles were within normal limits. Given the clinical suspicion of a submucosal neoplasm, the patient was taken up for direct laryngoscopy with micro laryngeal excision using CO₂ laser. Meticulous dissection was performed to achieve complete removal of the deposits while preserving the integrity of the vocal ligament and adjacent mucosa. The histopathological examination revealed eosinophilic, amorphous, acellular deposits in the subepithelial stroma (Figure 3). Congo red staining demonstrated classic apple green birefringence under polarized light, confirming the diagnosis of amyloidosis (Figure 4).
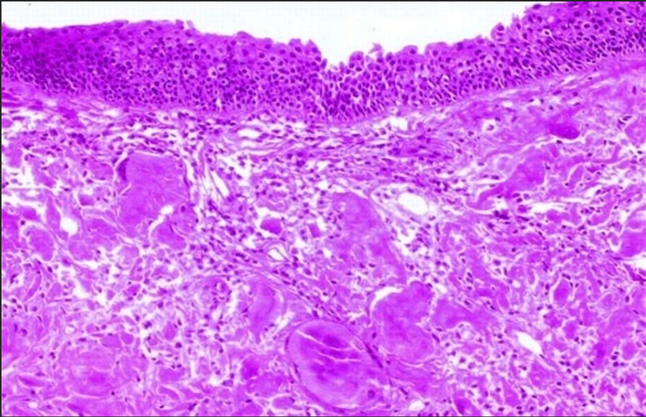
Figure 3. Histopathological examination showing respiratory epithelium with underlying pink amorphous debris
A subsequent systemic work-up including serum protein electrophoresis, urine Bence-Jones protein assay, echocardiogram and abdominal fat pad biopsy was initiated to exclude systemic amyloidosis. This established the final diagnosis of primary localized laryngeal amyloidosis.
The patient’s post-operative recovery was uneventful. A significant improvement in her voice quality was noted at 4 weeks follow-up and she remains free of recurrence with satisfactory phonatory outcomes till date (Figure 5).
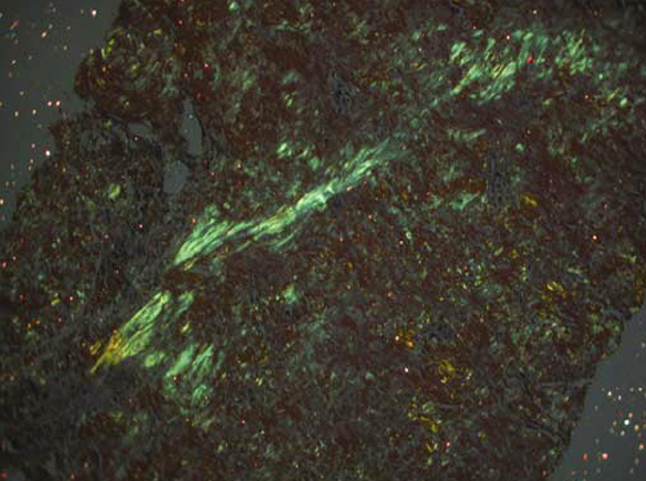
Figure 4. Image showing apple green birefringence under polarised light confirming amyloidosis
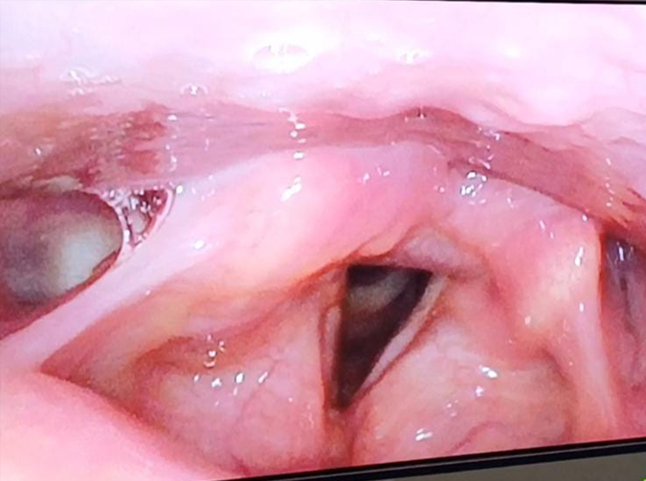
Figure 5. Follow-up videolaryngoscopic image done after 1 year showing no recurrence/residual lesion
Discussion
Laryngeal amyloidosis is a rare clinical entity whose aetiopathogenesis remains incompletely understood. The majority of cases are of the AL (light chain) type, indicating localized monoclonal plasma cell dyscrasia within the laryngeal tissue.3,7 Although it most commonly affects males in their fifth to seventh decade of life, it can occur in any age group and in either sex.4,6 The vocal cords and supraglottic structures are particularly vulnerable due to their rich vascular supply and abundance of lymphoid tissue, factors believed to contribute to localized plasma cell dyscrasia.5,7 Unlike systemic amyloidosis, the localized form is typically not associated with underlying hematologic malignancies.3
The diagnosis of laryngeal amyloidosis is frequently delayed due to its nonspecific nature of presentation. Hoarseness, often the only symptom, is commonly mistaken for more prevalent conditions such as laryngitis, vocal strain or laryngopharyngeal reflux.2,6 As a result, patients are often managed conservatively before imaging or considering a biopsy. On laryngoscopy, the lesions may mimic more common findings like vocal polyps, granulomas, or neoplastic growths.4 Radiological investigations such as CT or MRI usually reveal submucosal soft tissue thickening without features that distinguish amyloidosis from other benign entities.8 The definitive diagnosis requires histopathological evaluation, with Congo red staining and the demonstration of apple green birefringence under polarized light being diagnostic.5,6 Although immunohistochemistry and mass spectrometry can help identify the specific amyloid type, these tests are generally unnecessary in isolated laryngeal cases.3,6
Management of laryngeal amyloidosis remains individualized due to the rarity of the condition and lack of standardized treatment algorithms. Surgical excision remains the mainstay of therapy for localised disease, aimed at complete removal of amyloid deposits while preserving laryngeal function. CO₂ laser excision is currently the preferred technique because of its precision, haemostatic effect and ability to spare surrounding tissue.1,5,9 Cold steel excision may be used in select cases but it carries a higher risk of postoperative scarring and bleeding.4 The surgical goal is complete removal of amyloid deposits while preserving the structural integrity and vibratory function of the vocal cords.11
A thorough systemic evaluation is crucial in all cases to rule out systemic amyloidosis. This typically includes complete blood count, erythrocyte sedimentation rate, serum and urine protein electrophoresis, echocardiography, abdominal fat pad biopsy, and, when necessary, bone marrow biopsy.6,7 Localized laryngeal amyloidosis rarely progresses to systemic disease, but failure to identify systemic involvement could significantly alter management and prognosis.3
Long-term follow-up is essential, as the recurrence rate can be as high as 30%.1,5 Regular laryngoscopic surveillance is recommended, especially in patients with multifocal or extensive involvement. There is currently no role for chemotherapy or radiotherapy in the management of isolated laryngeal amyloidosis unless systemic disease is confirmed.3,6
Recent technological advances have refined the diagnostic and surgical approach to this condition. High-resolution narrow band imaging (NBI) has shown potential in identifying subtle vascular patterns characteristic of laryngeal amyloidosis, aiding early detection.10 The use of laser-assisted micro flap techniques has enhanced the ability to preserve delicate vibratory tissues, especially in diffuse lesions.11 Emerging research into biomarkers such as serum free light chains and genetic profiling may allow for better prediction of recurrence and disease progression.12 Additionally, robotic micro laryngeal surgery and three-dimensional exoscopic visualization systems are gaining attention as adjuncts in managing anatomically complex or recurrent cases, offering enhanced precision and ergonomics for the surgeon.13
Conclusion
This case highlights the critical need to investigate patient with persistent and unexplained dysphonia for rare pathologies like amyloidosis. A high index of suspicion with an eye for characteristic features on clinical examination can help in early diagnosis. Laryngeal amyloidosis, although rare, is a treatable entity. Early diagnosis confirmed by histopathology, followed by precise surgical excision using tools like CO₂ laser, offers patients an excellent prognosis with good functional outcomes. Long term vigilant follow up remains essential to monitor for disease recurrence.
END NOTE
Author information
- Dr. Anita Elza Thomas, Junior Resident, Department of ENT, Government Medical College Kozhikode. E-mail: anitaelzathomas@gmail.com
- Dr. Sapna. S. Nambiar, Additional Professor, Department of ENT, Government Medical College Kozhikode
E-mail: snambiar125@gmail.com - Dr. Hasila Beegum, Junior Resident, Department of ENT, Government Medical College Kozhikode
E-mail: hasilabeegumks@gmail.com - Dr. Amina Rajan, Junior Resident, Department of ENT, Government Medical College Kozhikode
E-mail: aminarajan19@gmail.com
Financial support: This work received no specific grant from any funding agency or commercial entity.
Conflict of Interest: None declared
References
- Bhujel K, Bhowmick N, Gandhi S, Sharma H, Mishra D. Primary laryngeal amyloidosis and CO2 laser as the treatment modality. Bengal J Otolaryngol Head Neck Surg. 2021;29(2):120–126.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=10.47210/bjohns.2021.v29i2.437.
[Crossref] 10.47210/bjohns.2021.v29i2.437 - Yiotakis I, Georgolios A, Charalabopoulos A, et al. Primary localized laryngeal amyloidosis presenting with hoarseness and dysphagia: a case report. J Med Case Rep. 2009;3:9049.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=10.4076/1752-1947-3-9049
[Crossref] 10.4076/1752-1947-3-9049. - Mesolella M, Petruzzi G, Buono S, et al. Focus on localized laryngeal amyloidosis: management of five cases. Open Med (Wars). 2020;15(1):327–332.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=10.1515/med-2020-0400
[Crossref] 10.1515/med-2020-0400. - Gonzalez M, Lajud S, Garraton F, Pacheco P. Laryngeal amyloidosis concealing carcinoma in situ: a management dilemma. Otolaryngol Case Rep. 2021;20:100310.
[PubMed[ https://pubmed.ncbi.nlm.nih.gov/?term=10.1016/j.xocr.2021.100310
[Crossref] 10.1016/j.xocr.2021.100310. - Salman R, Lateef M, Iqbal I, Rehman A, Islam M. Laryngeal amyloidosis: a case report. Indian J Otolaryngol Head Neck Surg. 2011;63(1):85–86.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=10.1007/s12070-010-0066-9
[Crossref] 10.1007/s12070-010-0066-9. - Zainol S, Azman M, Muthusamy S. Isolated laryngeal amyloidosis: a case report. Egypt J Otolaryngol. 2018;34(4):359–362.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=10.4103/ejo.ejo_12_18
[Crossref] 10.4103/ejo.ejo_12_18. - Villagómez-Ortiz VJ, Villegas-González M, Treviño-González JL, et al. Laryngeal amyloidosis: an uncommon cause of dysphonia. Med Univ. 2014;16(64):129–132.
[Pubmed] https://pubmed.ncbi.nlm.nih.gov/?term=10.1016/j.rmu.2014.01.003
[Crossref] 10.1016/j.rmu.2014.01.003. - Abdel Tawab HM, Sulaiman IA. Localized subglottic laryngeal amyloidosis: a case report. Egypt J Otolaryngol. 2018;34(4):337–340.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=10.4103/ejo.ejo_74_17
[Crossref] 10.4103/ejo.ejo_74_17. - Behnoud F, Baghbanian N. Isolated laryngeal amyloidosis. Iran J Otorhinolaryngol. 2013;25(70):49–50.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=Isolated+laryngeal+amyloidosis+Behnoud - Puxeddu R, et al. Narrow band imaging in laryngeal amyloidosis. Acta Otorhinolaryngol Ital. 2021;41(1):63–68.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=Narrow+band+imaging+laryngeal+amyloidosis - Galli J, et al. CO2 laser-assisted microflap in the treatment of laryngeal amyloidosis. Eur Arch Otorhinolaryngol. 2022;279(5):2171–2175.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=CO2+laser+microflap+laryngeal+amyloidosis - Oba T, et al. Amyloidosis of the larynx: clinical features and risk of recurrence. Laryngoscope. 2020;130(8):1898–1903.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=Amyloidosis+of+the+larynx+Oba - Yoon JH, et al. Three-dimensional exoscopic surgery for laryngeal amyloidosis: a novel approach. J Voice. 2023;37(2):e149–e154.
[PubMed] https://pubmed.ncbi.nlm.nih.gov/?term=Three-dimensional+exoscopic+surgery+laryngeal+amyloidosis