Case Report Published on December 26, 2025
A Case Report on Synovial Sarcoma
Anjali Gangadharan1, Lini Joseph1, Sandeep Sreedhar1, P Muraleedharan Nampoothiri1
- Department of ENT, Malabar Medical College, Kozhikode*
Corresponding Author: Dr Anjali Gangadharan, Post Graduate
Department of ENT, Malabar Medical College, Kozhikode
Email: anjaligangadharan3@gmail.com
ABSTRACT
Introduction: Synovial sarcoma is a high-grade, spindle cell neoplasm of mesenchymal origin. We aim to document an unusual case of Synovial sarcoma of Ethmoid sinus, its clinical picture, diagnosis and management.
Case Report: A lady who presented with nasal block and watering eyes since 9 months. Nasal endoscopy revealed a bleeding polypoidal mass with CT evidence of adjacent bony erosions with intracranial extension. Biopsy revealed spindle cell neoplasm with specific immunohistochemical markers towards synovial sarcoma.
Conclusion: Synonasal synovial sarcoma presents similar to any benign sinonasal mass making diagnosis very difficult.To achieve a surgical clearance in the head and neck region can be challenging due to inaccessibility and proximity of vital structures. In our patient we performed wide excision of tumour via open approach followed by adjuvant treatment.
Keywords: Synovial Sarcoma, Sinonasal Malignancy, Spindle Cell Neoplasm, Lateral Rhinotomy, Ethmoid Sinus
INTRODUCTION
Synovial sarcoma is a high-grade, spindle cell neoplasm of mesenchymal origin. It derived its name from the microscopic resemblance of tumour cells to synoviocytes. Both sexes are equally affected.More common in third decade of life.1
The five-year survival rate is 47-58% with high incidence of recurrence. Most sarcomas occur in lower extremities, only 10% cases occur in head and neck region. In head and neck, parapharynx is the most common, followed by nasopharynx and oropharynx.2
Synovial sarcomas of paranasal sinus are extremely rare. Here we aim to document an unusual case of Synovial sarcoma of Ethmoidal sinus, its clinical picture, diagnosis and management.
CASE REPORT
A 61year old women (Figure 1) presented to our ENT out-patient department (OPD) with complaints of bilateral nasal obstruction and epiphora left eye for 9 months. Her nasal obstruction was insidious in onset. There was no history of associated symptoms like nasal discharge, epistaxis, postnasal drip, fever or headache.

Figure 1. Image of patient at the time of presentation
Anterior rhinoscopy showed a pinkish mass with regular, smooth surface filling the entire left nasal cavity and pushing the nasal septum to opposite side. Palpation revealed a friable mass with contact bleeding.
She had left eye proptosis with eye ball displaced laterally. Her visual acuity and eye movements were normal in all directions. Light reflex was present without relative afferent pupillary defect or papilloedema.
CT Paranasal sinus and Contrast MRI revealed a heterogeneously enhancing lesion located in the left nasal cavity and anterior ethmoid sinus extending superiorly till cribriform plate and fovea ethmoidalis, medially displacing nasal septum to right side and laterally compressing on lamina papyracea and medial rectus muscle with globe displaced anteriorly. No definitive intraconal or intracranial extensions were seen (Figure2 A &B).
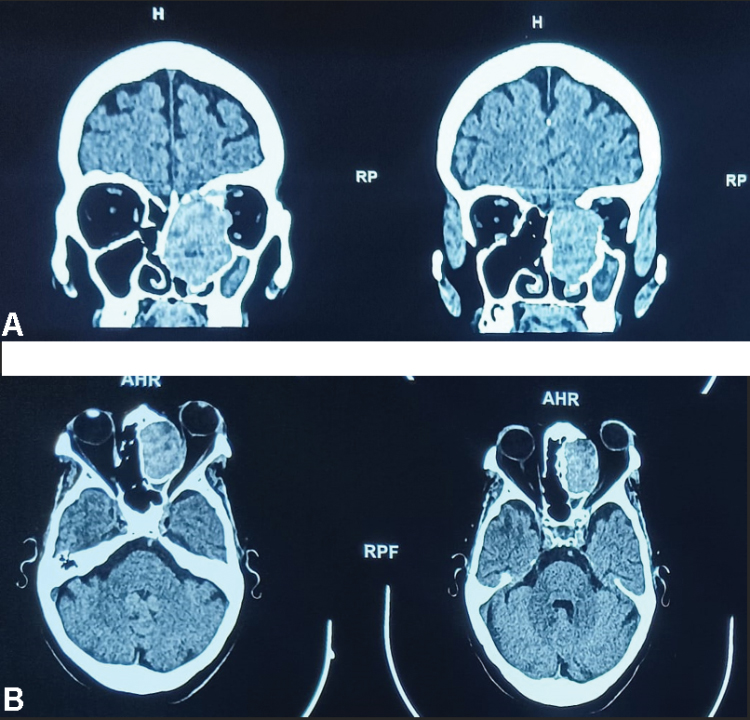
Figure 2. Contrast-enhanced CT coronal(A) and axial(B) images of nose and
paranasal sinuses showing heterogeneously enhancing lesion in left nasal cavity and
anterior ethmoidal sinus. Superiorly extending fovea ethmoidalis and cribriform
plate with septum being pushed to opposite side and lesion compressing medial rectus and lamina papyracea.
We then proceeded with diagnostic nasal endoscopy (DNE) and biopsy under general anaesthesia. Histopathology examination (HPE) showed malignant spindle cell neoplasm. As per AJCC classification (9th edition) tumour was staged as T4aNoMo.
Patient’s clinical, radiological, and pathological results were reviewed in a multidisciplinary tumour board, and a consensus decision was made to proceed with surgical intervention followed by adjuvant chemoradiotherapy (CRT), as recommended by medical oncology, radiation oncology and neurosurgery teams.
A wide excision of tumour was performed via a lateral rhinotomy approach with a Lynch-Howarth extension. The surgical procedure included complete external ethmoidectomy and tumour removal. The excised tumour specimen was sent for HPE. The postoperative period was uneventful.
Adjuvant CRT was initiated postoperatively. The regimen consisted of a combination of 2g/m2of Ifosfamide for three consecutive days and 75mg/m2 of Adriamycin divided over two days along with Mesna. Total 6 cycles of chemotherapy were given 21 days apart. Radiotherapy of 50 Gy was administered over a period of 5 weeks in 2 Gy fractions. The patient tolerated adjuvant chemoradiation well, and no complications were encountered.
The patient was followed up every 2 weeks for 2 months post-discharge, then monthly for 6 months in the ENT and Neurosurgery OPD. During follow up visits, her symptoms were assessed and DNE and suction clearance of nasal cavity was done. There were no recurrences or complications. She is now being followed up every 2 months for the next 6 months, after which she will transition to yearly follow-ups.
DISCUSSION
Synovial sarcoma is a rare and aggressive malignant tumour of soft tissue origin. Sinonasal synovial sarcoma typically presents with site-specific symptoms, but its rapid growth can lead to severe and potentially devastating complications, such as vision loss, if prompt diagnosis and treatment are not initiated.2
The exact aetiology is unknown, but radiation exposure has been linked to an increased risk of developing this tumour. Molecularly, synovial sarcoma is characterised by specific chromosomal translocations leading to the formation of fusion genes SY18-SSX. The origin of these translocations is still unknown, and further research is needed to understand the underlying mechanisms.2,3,4
The clinical presentation of synovial sarcomas can be similar to other tumours like, Frontoethmoidal mucoceles, Inverted papilloma, Rhabdomyosarcoma or Olfactory neuroblastoma. Immunohistochemical (IHC) analysis plays a crucial role in differentiating these tumours. IHC analysis of our study showed tumour cell reactivity towards CD99, Bcl2, S100 and TLE1 (Figure 3 B, C and D) which were the markers observed in studies conducted by Saklani P et al and Saito S et al suggestive of Biphasic synovial sarcoma.1,5,6
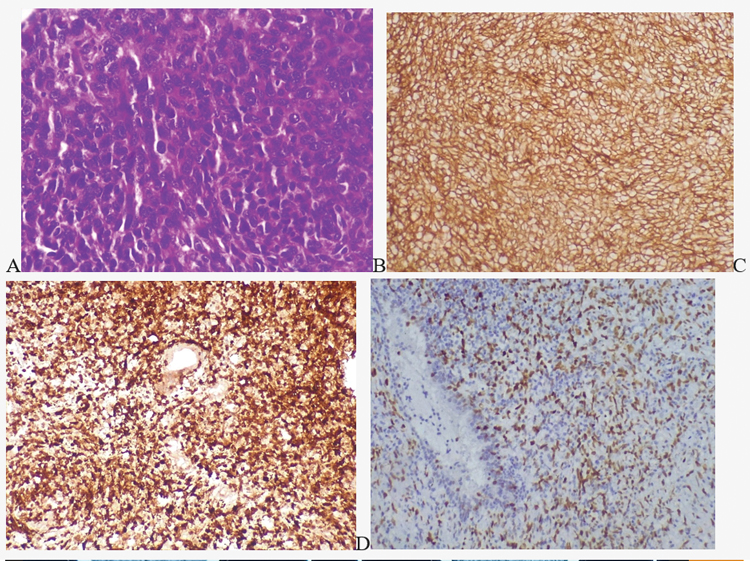
Figure 3. (A)H&E stain image showing atypical spindle cells with scanty cytoplasm, vesicular nucleus and prominent nucleoli. IHC staining positive to CD99 (B) BCl2 (C) and TLE1 (D
In studies conducted by Ayyasamy et al, Almahdi et al, Saito S et al and Dhiman S et al, the presenting complaints were similar to that of our study, however an additional symptom of hyposmia was noted in studies done by Ayyasamy et al and Almahdi et al.
Investigations used were CECT and preoperative biopsy in all the existing studies in the literature, which helped them to assess tumour extent, bone erosion, intracranial and orbital involvement, and tumour morphology, guiding management decisions and were consistent with our study.
Almahdi et al studied a 46-year-old patient who underwent a radical surgery as Anterior cranial fossa tumour resection and skull base reconstruction followed by postoperative CRT. No recurrence was noted in their 1-year follow-up period.
In contrast, Dhiman S et al reported a case, where an endoscopic approach was utilized; however, they mentioned that complete tumour clearance was not possible with microdebrider-assisted endoscopic approach due to proximity with vital structures like orbit, optic nerve and dura. Even though they initiated postoperative CRT, the patient developed recurrence after 6months, necessitating a salvage surgery, which included Anterior cranial fossa clearance and orbital exenteration.
Thus, an open surgical approach offers significant benefits and advantages. However, achieving this in the head and neck region can be challenging due to the inaccessibility and proximity of vital structures. Wide surgical resection in this area can lead to significant cosmetic and functional impairment, necessitating a multimodal approach in advanced cases. In our study, we used a less radical approach to reduce functional morbidity and provide improved quality of life for the patient. Postoperative CRT was given to our patient, which was similar to other studies 4,6,7
Tumour size >5cm, high grade, margin positivity, location and depth of tumour are factors contributing for poor survival. Tumour size and margin could not be accurately assessed as extensive bony resection was avoided in our patient to avoid significant morbidity. A minimum of 5-year surveillance is needed for synovial sarcoma, and our patient was followed up for 1 year and showed no recurrence till now.8
CONCLUSION
The rarity of sinonasal synovial sarcomas poses diagnostic challenges due to the limited studies on it. Early diagnosis with a combination of DNE, imaging and HPE with IHC aids in diagnosis and a multimodal treatment is necessary for effective disease clearance, which includes surgical resection and adjuvant CRT. Long-term surveillance is crucial to monitor recurrences and ensure optimal patient outcomes.9
END NOTE
Author information
- Dr Anjali Gangadharan, Post Graduate,
Department of ENT, Malabar Medical College
Email: anjaligangadharan3@gmail.com - Dr Lini Joseph, Assistant Professor,
Department of ENT, Malabar Medical College
Email: linijomedico@gmail.com - Dr Sandeep Sreedhar, Professor,
Department of ENT, Malabar Medical College
Email: sreedhar.sandeep@gmail.com - Dr P Muraleedharan Nampoothiri, Professor & HOD,
Department of ENT, Malabar Medical College,
Email: pmnamboothiri@yahoo.com
Financial Support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors
Ethical Standard: Written informed consent was obtained from the patient for publication of this case report and accompanying images. Ethics committee approval was obtained for this case report as per institutional guidelines.
REFERENCES
1. Ayyaswamy A, Lakshmanan S, Manimaran V, Iyyasamy B. A case report on paranasal synovial sarcoma: rare tumor at an uncommon location. Int J Head Neck Surg. 2023;14(3):51-3
2. Almahdi M, ALHumaid SA, Alsafi M, AlObaid F, Alsalim A. Nasal spindle cell sarcoma: a case report. Int J Surg Case Rep. 2020;72:515-9.
[PubMed]
3. Kumar V, Abbas AK, Aster JC. Robbins & Cotran pathologic basis of disease. 1st Bangladesh ed. Philadelphia: Elsevier Health Sciences; 2017
4. Harb WJ, Luna MA, Patel SR, Ballo MT, Roberts DB, Sturgis EM. Survival in patients with synovial sarcoma of the head and neck: association with tumor location, size, and extension. Head Neck. 2007;29(8):731-40.
[Pubmed]
5. Saklani P, Shetageri SN, Parthiban SRR. Sinonasal synovial sarcoma masquerading as a common soft tissue tumor: a diagnostic challenge and literature review. J Med Sci Health. 2022;8(3):292-5.
6. Saito S, Ozawa H, Ikari Y, Nakahara N, Ito F, Sekimizu M, et al. Synovial sarcoma of the maxillary sinus: an extremely rare case with excellent response to chemotherapy. Onco Targets Ther. 2018;11:483-8.
[PubMed]
7. Dhiman S, Negi S, Moudgil S, Thakur JS, Azad RK. Synovial Sarcoma of Ethmoidal Sinus. Surg J (N Y). 2021 Aug 3;7(3):e195-e198.
[Pubmed]
8. Watkinson JC, Gilbert RW. Stell and Maran’s Textbook of Head and Neck Surgery and Oncology. 5th ed. London: Hodder Arnold; 2012.
9. Gore MR. Treatment, outcomes, and demographics in sinonasal sarcoma: a systematic review of the literature. BMC Ear Nose Throat Disord. 2018;18:1