Original Research Published on December 26, 2025
Coblator-Assisted Partial Glossectomy with Neck Dissection in Oral Tongue Carcinoma : A Safe and Function Preserving Surgical Technique
Sahir N Abdulla1, Padmakumar J2, Sandeep Saseendran1, R Praseeda Prasad1, Sruthi Ramakrishnan K1, Abdul Basith3
- Department of Otolaryngology and Head & Neck Surgery, PRS Hospital, Thiruvananthapuram; 2. Department of Plastic Surgery, PRS Hospital, Thiruvananthapuram; 3. Department of ENT, Sri Siddhartha Medical College, Tumkur, Karnataka*
Corresponding Author: Dr Sandeep Saseendran
Consultant in ENT, Department of Otolaryngology and Head & Neck Surgery, PRS Hospital, Trivandrum Email- ssathiyadam@gmail.com
ABSTRACT
Background: Oral tongue squamous cell carcinoma (OTSCC) is a prevalent malignancy in India. Conventional surgical techniques, while effective, can be associated with significant morbidity. Coblation technology offers precise tissue dissection with minimal thermal damage, potentially improving functional outcomes.
Objective: To evaluate the safety, oncological adequacy, and functional outcomes of coblator-assisted partial glossectomy with neck dissection in early-stage OTSCC.
Methods: A prospective observational study was conducted on 15 patients (T1-T2, N0-N1). All underwent coblator-assisted partial glossectomy with neck dissection. Intraoperative parameters (blood loss, operative time, margin status), postoperative recovery (pain, oral intake resumption), functional outcomes (speech, swallowing), and oncological results were assessed.
Results: The mean intraoperative blood loss during glossectomy was 23.4 mL. All patients achieved clear surgical margins. Postoperative pain was low (mean VAS 3.1 on Day 1), and oral intake resumed early (mean 2.1 days). Speech and swallowing functions were well-preserved. No major complications or locoregional recurrences were observed over a 24-month follow-up.
Conclusion: Coblator-assisted partial glossectomy is a safe and effective technique for early OTSCC, offering reduced blood loss, favourable functional recovery, and sound oncological outcomes. It represents a promising function-preserving surgical alternative.
Keywords: Carcinoma, Squamous Cell, Glossectomy, Neck Dissection, Radiofrequency Ablation, Tongue Neoplasms, Treatment Outcome
Introduction
Carcinoma of the oral tongue is one of the most prevalent and biologically aggressive malignancies of the oral cavity, particularly in the Indian subcontinent, contributing to a substantial portion of global oral cancer cases.1 India accounts for nearly one-third of the world’s oral cancer burden, and oral tongue squamous cell carcinoma (OTSCC) has shown a rising incidence, including among younger adults.2 This increased prevalence is strongly associated with the widespread use of tobacco in various forms, alcohol consumption, and betel nut (areca nut) chewing, which are culturally ingrained habits in many parts of India.3,4 Chronic mechanical irritation from sharp teeth is also recognized as a contributing etiological factor in the development of OTSCC in Indian patients.5
The extensive lymphatic network of tongue predisposes patients to early cervical nodal metastasis, making timely diagnosis and appropriate surgical intervention essential for disease control.6 Partial glossectomy with adequate margins, combined with appropriate neck dissection, remains the gold-standard treatment for early-stage OTSCC.7 Conventional surgical approaches, including cold steel scalpel and monopolar electrocautery, are effective but associated with limitations such as higher intraoperative blood loss, collateral thermal injury, and greater postoperative morbidity, which may delay functional recovery.8,9
Coblation (controlled ablation) technology utilises bipolar radiofrequency energy to create a plasma field that dissects tissue at relatively low temperatures (40–70°C), resulting in precise tissue removal with minimal thermal damage to surrounding structures.10 This advantage is particularly relevant for tongue surgery, where preservation of key functions such as speech, swallowing, mastication, taste, and airway protection is crucial for postoperative quality of life.11
Although coblation has gained popularity in various ENT procedures, including adenotonsillectomy and laryngeal surgeries, its application in oral tongue cancer remains under-reported within the Indian context.12 Preliminary studies suggest that coblation may reduce intraoperative bleeding, minimise postoperative pain, and improve early functional outcomes without compromising oncological safety.13 However, further clinical evidence is required to validate its efficacy in achieving oncologically sound resections with improved recovery.
This study aims to evaluate the safety, oncological adequacy, and functional outcomes of coblator-assisted partial glossectomy with neck dissection in patients with early-stage OTSCC, with a focus on intraoperative blood loss, patient recovery, and preservation of speech and swallowing.
Literature Review
Epidemiology and Risk Factors
Oral tongue cancer represents 16–30% of all oral cavity malignancies in India, a higher proportion compared to Western countries.2,3 The strong cultural prevalence of tobacco in smoked and smokeless forms, alongside alcohol and areca nut consumption, significantly contributes to carcinogenesis.3,4 Younger age onset, increasingly reported in recent decades, has been linked to early initiation of areca nut and tobacco use.2 Chronic mechanical irritation from sharp or mal-aligned teeth is also recorded as a risk factor.
Surgical Management of Early Oral Tongue Carcinoma
Margin-clear surgical resection remains the primary treatment modality for early-stage OTSCC.7 A minimum of 1 cm gross surgical margin is generally recommended to achieve histologically safe tumour-free margins.14 Elective neck dissection is often indicated even in clinically node-negative (cN0) cases due to the high incidence of occult nodal metastasis.6 While scalpel excision offers good histological margin clarity, it is associated with significant intraoperative bleeding.8 Electrocautery provides effective hemostasis but causes deeper thermal tissue injury, leading to increased post-operative pain, oedema and delay in regaining tongue mobility and oral intake.9
Coblation in Oral and Head–Neck Surgery
Coblation has been widely used in ENT surgeries such as tonsillectomy, turbinate reduction, adenoidectomy, and laryngeal procedures due to its ability to achieve precise ablation with reduced thermal damage.10,12 In oral cavity surgery, including glossectomy, coblation has shown advantages such as reduced bleeding, better intraoperative visibility, minimal muscle fiber damage, and improved preservation of neurovascular structures.11,13
Coblation vs Conventional Techniques in Tongue Resection
Comparative studies evaluating coblation, scalpel, and electrocautery techniques have demonstrated several benefits with coblation in tongue surgery. These include reduced intraoperative blood loss,13 reduced postoperative pain, faster wound healing, and earlier return to oral feeding and articulation.11,13 Reduced lateral thermal spread associated with coblation contributes to better postoperative tongue mobility and improved functional outcomes, aiding in faster rehabilitation.10,11
Functional Outcomes and Quality of Life
Essential role of tongue includes speech, swallowing, mastication, and airway protection. Preservation of these functions is integral to postoperative quality of life.11 Reduced tissue trauma and postoperative inflammation associated with coblation facilitate earlier return to oral intake, improved speech clarity, and better swallowing outcomes, thereby enhancing overall quality of life.13
Gaps in Literature
Despite promising evidence, research specifically evaluating coblation-assisted glossectomy for tongue cancer in India is limited.12 High-quality prospective studies assessing intraoperative, oncological, and functional outcomes are required to establish coblation as a standard adjunct in the surgical management of OTSCC.14
Aim and Objectives
Aim
• To evaluate the efficacy, oncological safety, and functional outcomes of coblator-assisted partial glossectomy with neck dissection in patients diagnosed with oral tongue squamous cell carcinoma.
Objectives
The objectives of this study are:
1. To assess intraoperative outcomes
• Operative time
• Estimated blood loss
• Surgical margin status
2. To evaluate postoperative recovery parameters
• Postoperative pain scores
• Duration of hospital stay
• Time to resume oral intake
• Postoperative complications
3. To analyse functional outcomes following surgery
• Speech clarity
• Swallowing function
4. To determine oncological effectiveness of the procedure
• Adequacy of lymph node clearance
• Local and regional disease control
• Recurrence rates during follow-up
Materials and Methods
Study Design
This study was designed as a prospective observational study conducted on patients diagnosed with oral tongue squamous cell carcinoma who underwent coblation-assisted partial glossectomy with neck dissection.
Study Setting and Duration
The study was carried out in the Department of Otorhinolaryngology at a tertiary care centre. Data collection, surgery, and follow-up were conducted over a period of 24 months.
Study Population and Sample Size
A total of 15 patients fulfilling the eligibility criteria were included in the study. The study population consisted of 10 males and 5 females between 30 and 70 years of age.
Inclusion Criteria
• Patients diagnosed with primary oral tongue squamous cell carcinoma (T1–T2).
• Clinical nodal status N0 or N1.
• Patients undergoing partial glossectomy with neck dissection using coblation.
• Patients willing to provide informed consent and comply with follow-up.
Exclusion Criteria
• Recurrent or residual tongue malignancy.
• Previous radiotherapy or chemotherapy to the head and neck region.
• Evidence of distant metastasis at presentation.
• Patients medically unfit for surgery.
Pre-operative Evaluation
All patients underwent a detailed clinical history and examination, including assessment of tobacco, alcohol, betel nut usage, and chronic mechanical trauma such as sharp teeth or dental prosthesis. Routine blood investigations, imaging with contrast-enhanced CT or MRI of the oral cavity and neck, and pre-anaesthetic evaluation were conducted. Biopsy confirmation of squamous cell carcinoma was mandatory prior to surgery.
Surgical Technique
Coblation-Assisted Partial Glossectomy
Surgery was performed under general anaesthesia. The extent of glossectomy was planned based on tumour size and location, ensuring adequate resection margins (Figure 1). The coblation system was used for mucosal incision and tumour excision. Tissue resection was carried out with controlled plasma-mediated ablation, allowing precise dissection with minimal thermal injury. Intraoperative haemostasis was achieved using the coagulation mode of the coblation device. Resection margins were labelled and sent for histopathological examination.

Figure 1. Ulceroproliferaive lesion left lateral border of tongue
Neck Dissection
Neck dissection was performed based on clinical and radiological nodal status. Selective neck dissection of Levels I–IV was carried out in cases with N0 or limited N1 disease, while modified radical neck dissection (MRND) was performed for clinically significant nodal involvement. Care was taken to preserve vital neurovascular structures where feasible.
Parameters Assessed
The following parameters were evaluated:
Intraoperative:
• Operative time
• Estimated blood loss
• Surgical margin status
Postoperative:
• Pain scores assessed using the Visual Analogue Scale (VAS)
• Duration of hospital stay
• Time to resume oral intake
• Postoperative wound-related or systemic complications
Functional Outcomes:
• Speech clarity
• Swallowing function
Oncological Outcomes:
• Lymph node yield
• Local and regional disease control
• Recurrence during follow-up
Follow-up Protocol
Patients were followed up at regular intervals: every 2 weeks for the first month, monthly for the next 6 months, and once every 3 months thereafter. Follow-up assessment included clinical examination, evaluation of functional outcomes, and surveillance for recurrence (Figure 2).

Figure 2. Ulceroproliferaive lesion left lateral border of tongue
Statistical Analysis
Data were recorded and analysed using standard statistical methods. Descriptive statistics were used for demographic and clinical variables. Continuous variables were expressed as mean and range, and categorical variables as frequency and percentage.
Results
Patient Demographics
A total of 15 patients diagnosed with early-stage oral tongue squamous cell carcinoma (T1–T2) were included in the study. The age of patients ranged from 30 to 70 years, with a mean age of 52.4 years. There were 10 males and 5 females, showing a male predominance (Figure 3). The most common predisposing factors identified were tobacco consumption (73%), followed by alcohol use (53%), betel nut chewing (47%), and chronic irritation from sharp teeth (27%) (Table 1).
Figure 3. Pie diagram Gender distribution
Tumour Characteristics
The majority of tumours were located on the lateral border of the anterior two‑thirds of the tongue. Six patients (40%) presented with T1 lesions, and nine patients (60%) presented with T2 lesions (Figure 4) (Table 2).
Intraoperative Parameters
Coblator-assisted partial glossectomy was successfully performed in all patients. The mean time taken for the glossectomy portion alone was 19.2 minutes for the overall cohort, with T1 cases averaging 18 minutes and T2 cases averaging 21 minutes (Table 3). The mean total operative time, including neck dissection, was 160 minutes. Intraoperative blood loss during the glossectomy using coblation was significantly low, averaging 23.4 mL (T1: 20.3 mL, T2: 25.8 mL). Total blood loss, including neck dissection, averaged 107 mL (Figure 5).
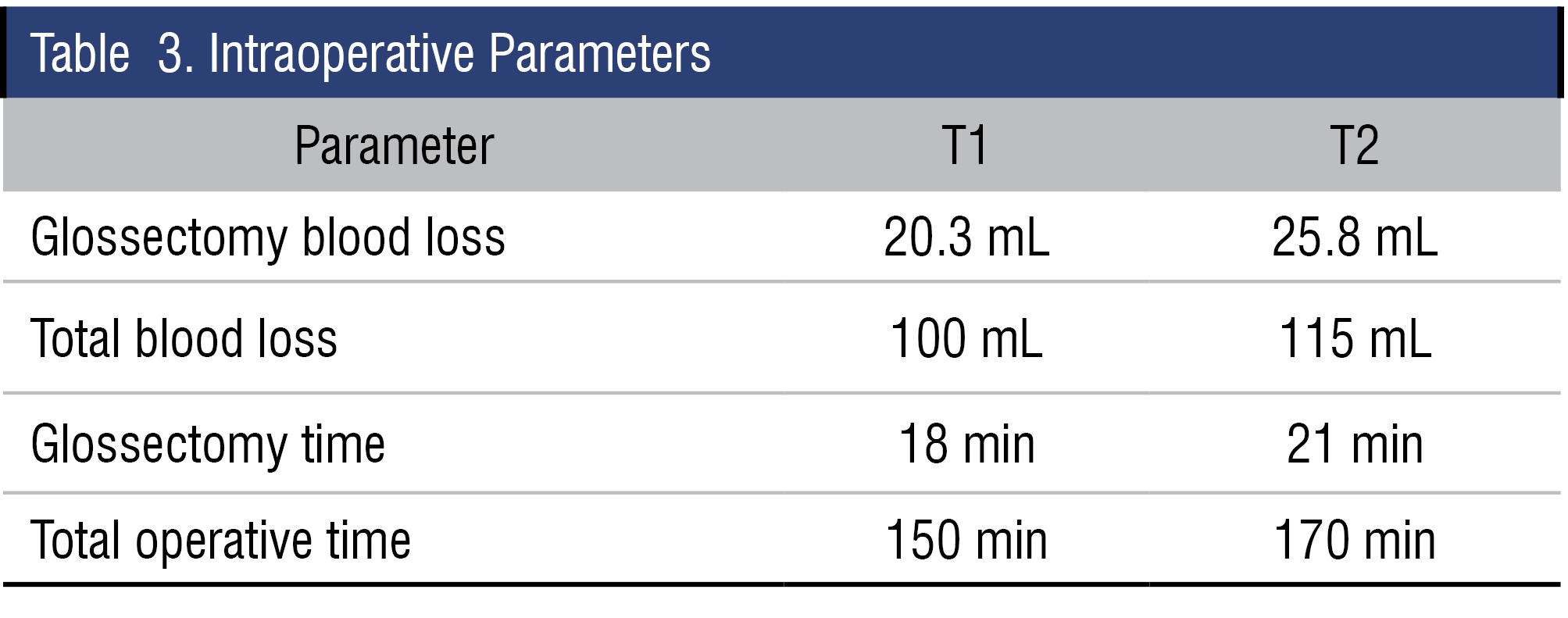
Figure 5. Bar diagram showing mean intra operative blood loss and operative time
Postoperative Outcomes
Patients demonstrated favourable postoperative recovery with minimal pain and early return to oral intake. The mean postoperative pain score on the Visual Analogue Scale (VAS) was 3.1 on Day 1, reducing to 1.2 by Day 3. The average time to resume oral feeding was 2.1 days, and most patients achieved normal speech clarity and swallowing within one week. Early tongue mobility was well preserved due to minimal thermal tissue damage.
Complications and Follow‑Up
No major postoperative complications such as flap necrosis, wound dehiscence, hematoma, airway compromise, or infection were observed. Minor tongue edema was seen in two patients, which resolved with conservative management. During the follow‑up period of 24 months, all patients remained disease‑free with no loco‑regional recurrence observed.
Discussion
Carcinoma of the oral tongue continues to represent a significant proportion of head and neck malignancies, with a well‑established propensity for early cervical lymphatic spread due to its rich submucosal lymphatic network. Surgical excision with adequate oncological margins remains the cornerstone of management and is often combined with neck dissection to address potential microscopic nodal disease. In recent years, newer surgical modalities such as laser and radiofrequency‑based instruments have been introduced to minimise collateral tissue damage and reduce morbidity. Among these, coblation has gained increasing attention due to its ability to ablate soft tissue at relatively low temperatures, thereby reducing thermal injury when compared with conventional monopolar electrocautery.
The present study demonstrates that coblation‑assisted partial glossectomy is a safe and effective technique for early‑stage oral tongue carcinoma, achieving oncologically sound resections with minimal morbidity. All patients in this study had clear surgical margins, supporting the precision associated with coblation‑based dissection. These findings correlate with previous studies reporting satisfactory oncological outcomes and adequate deep margin clearance using coblation for tongue lesions. Furthermore, minimal thermal artefact facilitated accurate histopathological margin assessment, which has been consistently highlighted in literature as an advantage of coblation.
A notable advantage in this study was reduced intraoperative blood loss during glossectomy. The mean blood loss was significantly lower than values commonly reported with cold steel dissection and electrocautery. Reduced bleeding enhances surgical field visibility, minimises need for suction, and facilitates precise dissection. Although total blood loss understandably increased when combined with neck dissection, the benefit of coblation during the primary tumour resection remained evident.
Functional outcomes are particularly relevant in oral tongue carcinoma due to the critical role of the tongue in speech, swallowing, and mastication. Patients in this study reported low postoperative pain scores and early resumption of oral intake, with most beginning soft diet within a few days. These findings align with earlier comparative studies where coblation‑based glossectomy showed reduced pain, decreased analgesic use, and faster return to normal diet when compared with electrocautery. Low operating temperatures reduce collateral neuromuscular damage, charring, and fibrosis, thereby aiding in preservation of tongue mobility and function.
The complication profile was favourable, with no major postoperative complications such as hematoma, wound breakdown, or airway issues. Only mild transient tongue oedema occurred in a few patients, which resolved with conservative management. No loco‑regional recurrence was noted during the 24‑month follow‑up, indicating satisfactory short‑term disease control. Although encouraging, long‑term follow‑up with larger cohorts is essential to validate oncological safety.
In the Indian context, particularly in Kerala, the high burden of oral cavity cancers is strongly linked to habits such as tobacco chewing, smoking, alcohol consumption, and areca nut use. Many patients in this study had one or more of these risk factors, consistent with regional epidemiological patterns. Coblation‑assisted glossectomy offers meaningful benefits in this setting by enabling faster postoperative recovery and better preservation of quality of life—crucial for younger, working‑age patients who form a significant proportion of tongue cancer cases in South India.
Despite these strengths, limitations exist. The study sample size was relatively small, and absence of a direct comparison group (electrocautery/cold steel) limited the ability to perform comparative statistical analysis. Operative time reflected total surgical duration including neck dissection, which may have masked the isolated time benefit attributable to coblation. A short learning curve is required for surgeons transitioning from conventional methods, but once familiarised, coblation offers improved operative precision. Cost considerations may influence adoption in resource‑limited settings, although reduced analgesic use, shorter hospital stays, and faster rehabilitation may balance costs.
In conclusion, this study adds to growing evidence supporting coblation‑assisted partial glossectomy as a function‑preserving alternative to conventional techniques for early‑stage oral tongue carcinoma. Reduced intraoperative blood loss, favourable functional recovery, and excellent early oncological outcomes underscore its clinical value. Given the high prevalence of tongue cancer and increasing emphasis on quality‑of‑life outcomes in India, coblation represents a promising addition to surgical practice. Larger multicentric trials with longer follow‑up are recommended to strengthen evidence for routine integration of coblation in tongue cancer surgery.
Summary and Conclusion
This study evaluated the role of coblation-assisted partial glossectomy combined with neck dissection in the management of early-stage oral tongue squamous cell carcinoma, with particular attention to blood loss, surgical efficiency, and preservation of oral functions. The procedure was performed in a group of patients aged between 30 and 70 years, with a male predominance and common exposure to regional risk factors such as tobacco, alcohol, areca nut chewing, and chronic mechanical trauma from sharp teeth.
Coblation-assisted tumor excision resulted in noticeably lower intraoperative blood loss during glossectomy when compared with figures reported for conventional techniques. Surgical resection was efficient, and all patients achieved clear margins, indicating oncological adequacy. Postoperative recovery was favorable, with most patients resuming oral intake earlier than usually expected following traditional methods. Pain levels were comparatively lower, and speech and swallowing functions were well preserved. No major postoperative complications were observed, and no locoregional recurrences were detected over the follow-up period.
In summary, coblation-assisted partial glossectomy appears to be a safe and effective method for the management of early oral tongue carcinoma. It provides distinct advantages in terms of surgical precision, reduced morbidity, and better functional outcomes. While the findings are promising, larger multicentric studies with longer follow-up are recommended before establishing coblation as a routine standard of care.
END NOTE
Author information
- Dr Sahir N Abdulla
HOD & Senior Consultant in ENT
Department of Otolaryngology and Head & Neck Surgery, PRS Hospital, Trivandrum
Email: drsahirsabdulla@yahoo.co.in - Dr Padmakumar J
Senior Consultant in Plastic Surgery,
Department of Plastic Surgery,
PRS Hospital, Trivandrum
Email: padmakumarjkurup@yahoo.co.in - Dr Sandeep Saseendran, Consultant in ENT, Department of Otolaryngology and Head & Neck Surgery, PRS Hospital, Trivandrum
Email: ssathiyadam@gmail.com - Dr. R Praseeda Prasad
Consultant in ENT, Department of Otolaryngology and Head & Neck Surgery
PRS Hospital, Trivandrum
Email: rpraseedaprasad@gmail.com - Dr Sruthi Ramakrishnan K
Consultant in ENT, Department of Otolaryngology and Head & Neck Surgery
PRS Hospital, Trivandrum
Email: sruthi.rk688@gmail.com - Dr Abdul Basith, Resident, Department of ENT,
Sri Siddhartha Medical College, Tumkur, Karnataka.
Email: basithzlon@gmail.com.
Financial Support: Nil
Conflict of Interest: None declared
References
- Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2009;45(4–5):309–316.
[PubMed] - Krishnamurthy A, Ramshankar V. Early onset oral tongue cancer among non-habitual young people: an increasing trend observed in a South Indian patient population. Indian Journal of Cancer. 2013;50(4):283–288.
- Gupta B, Johnson NW. Systematic review and meta-analysis of association of smokeless tobacco and alcohol with oral cancer in India. Indian Journal of Public Health. 2013;57(1):1–12.
- Gupta PC, Ray CS. Epidemiology of betel quid usage. Ann Acad Med Singap. 2004;33(4 Suppl):31–36.
[PubMed] - Shetty K, Khandige G, Khora SS. Association of chronic mechanical trauma and oral squamous cell carcinoma—A hospital-based study. J Oral Maxillofac Pathol. 2017;21(3):461–467.
[Pubmed] - Fakih AR, Rao RS, Borges AM. Elective versus therapeutic neck dissection in early carcinoma of the oral tongue. Am J Surg. 1989;158(4):309–313.
[PubMed] - National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology: Head and Neck Cancers. Version 1.2024.
- Byers RM. Squamous cell carcinoma of the oral tongue: clinical and pathologic considerations. Head Neck Surg. 1985;7(1):62–66.
[PubMed] - Buchanan MA, Cole D, Collyer J. Electrosurgery and surgical diathermy. Anaesthesia & Intensive Care Medicine. 2012;13(9):400–403.
- Myers EN, Ferguson CF. The use of coblation in otolaryngology–head and neck surgery. Operative Techniques in Otolaryngology–Head and Neck Surgery. 2002;13(1):3–10.
- Feng AL, Patel A, Bonilla-Velez J. Coblation technology in head and neck surgery: Benefits and applications. Current Opinion in Otolaryngology & Head and Neck Surgery. 2020;28(6):411–418.
- Babu SC, et al. Coblation-assisted tongue surgeries: A prospective clinical evaluation. Journal of Clinical and Diagnostic Research. 2017;11(3):MC01–MC04.
- Kumar N, Sharma R, Singh J. Comparative evaluation of coblation versus monopolar electrocautery in partial glossectomy for oral cancer. Journal of Oral and Maxillofacial Surgery. 2021;79(5):1010–1016.